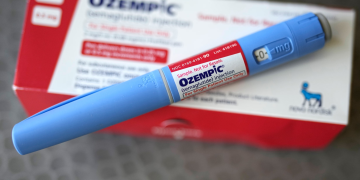
Ozempic is widely discussed for blood sugar and weight-related care. Many people are unsure how it works and what to expect day to day. For balanced reading, use trusted sources and speak with your healthcare team.
People hear many claims online; for clear, neutral background, see Ozempic (semaglutide) information which outlines dosing formats and general use, then discuss questions with your clinician. This article explains how the medication fits into overall care. It also reviews benefits, limits, and common challenges.
What Ozempic Is and How It Works
Ozempic contains semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist. GLP-1 is a natural hormone that helps regulate blood sugar and appetite. By mimicking GLP-1, the medication can help your body release insulin when glucose is high. It may also slow stomach emptying and reduce hunger for some people.
This effect can support type 2 diabetes management. It can also assist weight-related goals under medical supervision. Results vary, and it is not a cure for diabetes or obesity. It works best alongside nutrition, movement, sleep, and stress management.
Who Might Be Considered for Treatment
Type 2 diabetes often develops gradually. Early signs can include increased thirst, frequent urination, fatigue, and slow-healing cuts. Some people notice blurred vision or recurrent infections. Others have no symptoms until blood tests show elevated glucose or A1C.
Weight-related challenges can raise insulin resistance. This means the body’s cells respond less to insulin, making glucose control harder. Family history, stress, sleep loss, and some medications also contribute. A clinician may discuss GLP-1 therapy when lifestyle changes and other measures have not achieved targets.
Ozempic is not appropriate for everyone. Clinicians review medical history, current medicines, and personal risks. They also consider goals like A1C reduction, weight changes, and heart or kidney protection. Decisions are individualized and revisited over time.
Potential Benefits and Limits
Potential benefits include improved fasting and post-meal blood sugars. Some people also experience weight loss, which may reduce insulin resistance. Better glucose control can lessen symptoms like fatigue and thirst. It may also support long-term risk reduction when sustained.
Limitations are equally important. Not everyone loses weight or reaches glucose targets. Some experience side effects, especially when starting or increasing the dose. Adherence can be challenging, and results depend on consistent use and lifestyle support. Ongoing monitoring helps adjust the plan as needed.
Common Side Effects and Safety Considerations
Gastrointestinal effects are the most common. Nausea, vomiting, diarrhea, constipation, and decreased appetite can occur. These usually lessen as the body adjusts, especially with slower dose increases. Hydration and smaller, simpler meals can help.
Less common risks are discussed during prescribing. These may include gallbladder issues or pancreatitis, which involves inflammation of the pancreas. Very severe stomach pain, persistent vomiting, or signs of dehydration should prompt urgent evaluation. People with a history of certain endocrine tumors or pancreatitis may not be candidates.
Discuss all medicines and supplements with your clinician. Some combinations can increase side effects or change blood sugar patterns. If you use other diabetes medicines, watch for low blood sugar symptoms. These include shakiness, sweating, hunger, and confusion.
How Ozempic Fits Into a Broader Care Plan
Most people do best with a structured routine. Plan weekly grocery lists, meal prep, and set reminders for injections. Check blood glucose as recommended, especially during dose changes. Track symptoms, appetite, and bowel habits to share at checkups.
Nutritional patterns matter. Emphasize lean proteins, high-fiber vegetables, legumes, and whole grains. Choose unsweetened beverages and limit refined carbs and alcohol. Eat slowly and stop when comfortably full to reduce nausea.
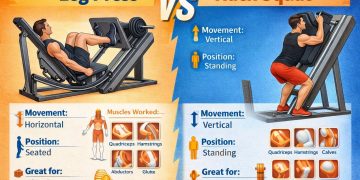
Movement supports insulin sensitivity. Aim for regular walking, cycling, or swimming. Start small if you are new to exercise, and add minutes gradually. Include strength training twice a week, as tolerated.
Sleep and stress also influence glucose and appetite. Target 7–9 hours of sleep. Try brief breathing exercises, stretching, or short walks after meals. Small, repeatable habits are more sustainable than strict plans.
What to Discuss With Your Clinician
Ask about starting dose, titration steps, and timing. Clarify what to do if you miss a dose or experience side effects. Review signs that require urgent care, such as severe abdominal pain or repeated vomiting. Agree on follow-up intervals and lab testing.
Talk through personal goals and trade-offs. For example, prioritizing A1C reduction, weight change, or minimizing side effects. Confirm how the medication interacts with your other treatments. Consider whether a GLP-1 is the right class for your needs.
If you want to understand the broader class, explore GLP-1 Agonists options and typical clinical uses with your provider. Class education can help set realistic expectations. It also clarifies how these medicines differ from insulin or other non-insulin therapies.
Practical Tips for Day-to-Day Use
Use a consistent injection day each week. Set two reminders: one the day before and one the day of. Rotate injection sites to reduce irritation. Thigh, abdomen, and upper arm are common areas.
Ease stomach symptoms with simple strategies. Eat smaller, more frequent meals. Favor bland, lower-fat foods during the first weeks. Sip fluids throughout the day to prevent dehydration.
Monitor patterns during dose changes. Log glucose readings, appetite, and GI symptoms. Share this log at your next appointment. Adjustments are normal and often improve comfort and outcomes.
Plan for travel and routines. Store pens as instructed, and pack supplies in carry-on. Keep a small snack if you use other medicines that can lower blood sugar. Build a backup plan for missed doses.
Recognizing When to Seek Care
Call your clinician if you cannot keep fluids down, feel faint, or have severe abdominal pain. Persistent vomiting, signs of gallbladder disease, or pancreatitis symptoms need urgent review. Report any unexplained lumps or neck swelling promptly. New or worsening vision changes also deserve quick attention.
Contact your healthcare team if you notice repeated low or high readings. Early adjustments can prevent complications. Bring your meter or app downloads to visits. Trends often guide safer, more precise changes.
Living With Diabetes and Weight Challenges
Progress is rarely linear. Expect weeks with plateaus, occasional setbacks, and wins. Focus on habits you can maintain for years, not days. Small, steady steps usually outlast rapid overhauls.
Support matters. Consider group classes, a registered dietitian, or diabetes education programs. Involve family or friends who respect your goals. Balanced routines support both physical and emotional health.
Key Takeaways
Ozempic can help manage blood sugar and support weight-related goals. It works best as part of a broader plan, including nutrition, movement, and sleep. Benefits and side effects vary, so personalized guidance is essential. Ongoing monitoring and open communication improve safety and outcomes.
For more diabetes and weight-management education and tools, explore resources from CanadianInsulin . Use these materials to inform discussions with your clinician and care team.
Medical disclaimer: This content is for informational purposes only and is not a substitute for professional medical advice.